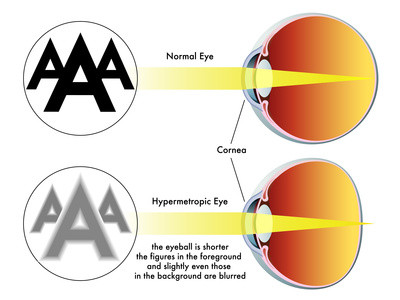
The onset of farsightedness can be late or early, depending on how severe the condition is. It usually begins at birth and gradually improves with age. The eye can accommodate for farsightedness through natural eye growth, but it can also be inherited. Although this condition is often genetic, it is also treatable and preventable. Read on to find out more about how to deal with this vision problem. For now, here are some tips to deal with it naturally.
The first step is to get regular eye exams to determine the extent of your farsightedness. The most reliable way to know whether you are farsighted or nearsighted is to visit your eye doctor for a thorough exam. Your optometrist will conduct a non-invasive eye examination that includes reading lines of letters on an eye chart and testing different lenses. A doctor will also measure the refractive error in your eyes and test the reflection from the rear of your eye.
The best way to treat farsightedness is to wear corrective lenses. A corrective lens is essential for farsighted people, especially those with other vision problems. However, there are many ways to treat it. Some of these methods include laser eye surgery or LASIK. These treatments can be expensive and require a prescription. Once you’ve been diagnosed with farsightedness, an optometrist will give you a prescription for glasses or contact lenses.
If left untreated, farsightedness may lead to eye strain, excess tearing, frequent blinking, and headaches. The condition can also impair reading and hand-eye coordination. Some people with this vision disorder do not even notice the blurring of their vision, as other parts of the visual system compensate for the lack of focus. Once your eyesight deteriorates, you will need to seek corrective lenses or surgery.
The best way to treat farsightedness is to wear contacts or glasses to correct your vision. It is important to see a doctor if you experience any vision problems, as they will be able to prescribe you with the best contact lenses. As farsightedness can cause problems with reading, it is important to see a doctor for further treatment. In addition to wearing contact lenses, your eye doctor will also check your eyesight to determine how much you are farsighted.
If you are farsighted, your eyes may experience pain and discomfort due to squinting. If you are nearsighted, you may suffer from severe eye strain and headaches. You may also experience blurred vision. If you are farsighted, you should see a doctor as soon as possible to get the right treatment. If your vision is worse than it should be, you may have corrective surgery to correct it.
Although farsightedness is usually an acquired condition, for some people it can last a lifetime. If you are very farsighted, your vision may deteriorate so much that you may lose your vision completely. The doctor can correct your vision. If you are farsighted, you will need to wear glasses or contact lenses until your vision is fully examined. This will correct your vision. But unless you are nearsighted, you may need to wear contact lenses.
A person who is farsighted is likely to have trouble reading objects. As a result, light reaches the retina, but the retina does not focus correctly. This results in blurred images. If you are farsighted, you will have difficulty reading. You will experience a wide range of vision problems, including nearsightedness and astigmatism. The site scots-westvirginia.org
explains that a good ophthalmologist will help you understand the causes and symptoms of vision problems and write the right prescription.
Although this condition is a common problem, it can still be corrected. In most cases farsightedness can be treated with glasses or contact lenses. Moreover, it is not a disease. In most cases, people with farsightedness have completely normal and healthy eyes. There are no complications from wearing glasses or contact lenses. There are also several types of glasses for children. If you are farsighted, you will need to wear them for close work.